| front |1 |2 |3 |4 |5 |6 |7 |8 |9 |10 |11 |12 |13 |14 |15 |16 |17 |18 |19 |20 |21 |22 |23 |24 |25 |26 |27 |28 |29 |30 |31 |32 |33 |34 |35|36 |37 |38 |39 |40 |41 |42 |43 |44 |45 |46 |47 |48 |49 |50 |51 |52 |53 |54 |55 |56 |57 |58 |59 |60 |61 |review |
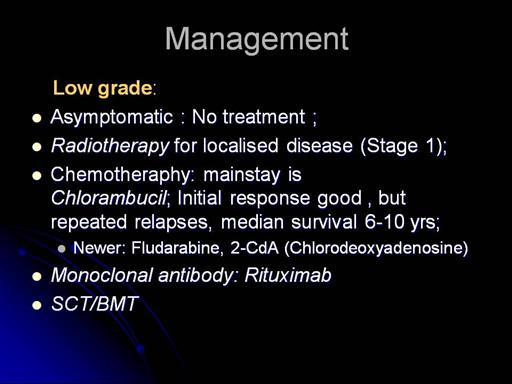 |
All cells have protein markers on their surface, known as antigens. Monoclonal antibodies are designed in the laboratory to specifically recognise particular protein markers on the surface of some cancer cells. The monoclonal antibody then 'locks' onto this protein. This either triggers the cell to destroy itself or signals to the body's immune system to attack and kill the cancer cell. For example, rituximab, the monoclonal antibody that is used in the treatment of non-Hodgkin's lymphoma, recognises a protein marker known as CD20. CD20 is found on the surface of the abnormal B cells that are found in some of the most common types of non-Hodgkin's lymphoma. When rituximab locks onto CD20 on the surface of a B cell, the cell may be destroyed directly, but also the body's natural defences are alerted. Rituximab effectively targets the lymphoma cells for destruction by the body's immune system, which can now kill the cancer cells. CD20 is also found on the surface of normal B cells, one of the types of white blood cells that circulate in the body. This means that these normal B cells, too, may be destroyed when rituximab is used. However, the stem cells in the bone marrow that develop into B cells do not have CD20 on their surface. Stem cells are therefore not destroyed by rituximab and can go on to replenish the body with healthy B cells. Although the number of mature, normal B cells is temporarily reduced by the treatment, they return to previous levels after the treatment. |