| front |1 |2 |3 |4 |5 |6 |7 |8 |9 |10 |11 |12 |13 |14 |15 |16 |17 |18 |19 |20 |21 |22 |23 |24 |25 |26 |review |
 |
1.Dawn
Phenomenon:
Hormones (growth hormone, cortisol, and catecholamines) produced by the body cause the liver to release large amounts of glucose into the bloodstream. These hormones are released in the early morning hours. These hormones also may partially block the effect of insulin, whether it's insulin your body produces or insulin from the last injection. If the body doesn't produce enough insulin blood sugar levels may rise. This may cause high blood sugar in the morning before the person eats.
2. Somogyi: Can occur when a person takes long-acting insulin for diabetes. Somogyi is caused by having too much insulin in the blood during the night. If the blood sugar level drops too low in the early morning hours, hormones (such as growth hormone, cortisol, and catecholamines) are released. These help reverse the low blood sugar level but may lead to blood sugar levels that are higher than normal in the morning. A person's body responds to the low blood sugar by causing a high blood sugar level in the early morning.
3.Hypoglycemia:
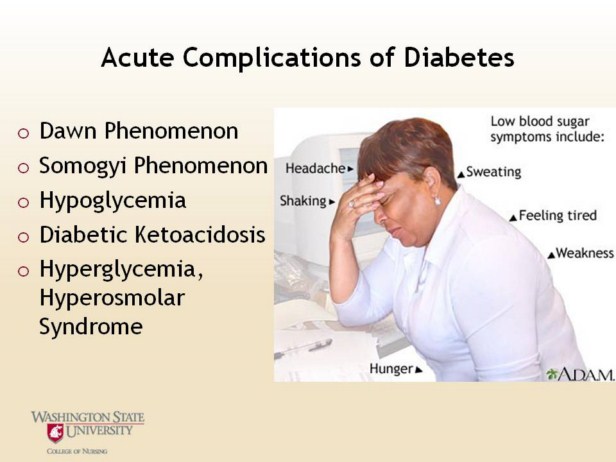
Hypoglycemia is one of the most common acute complications of diabetes and needs immediate treatment. Treatment includes testing to see where your blood sugar is and treating with 15 grams of a quick acting carbohydrate, such as juice, regular soda pop, glucose tablets, milk or glucose gel. Wait 15 minutes, test again and treat til the blood glucose is above 100. Instruct your patient that if they are going to eat within 45 minutes, then wait to eat, but if the next meal is more than 1 hour away, then have a snack of a protein and carbohydrate. Be sure to keep track of the pattern of when the low blood sugars are so that changes can be made to the patientís routine. Hypoglycemia is classified as either neuroglycopenic or neurogenic. Neuroglycopenic: shortage of glucose in the brain. Central nervous system deprivation Defects in hormonal counter regulation so delay or diminish the onset of autonomic symptoms, resulting in reduced hypoglycemic symptoms awareness. Neurogenic: or autonomic symptoms are the result of the perception of physiological changes caused by the central nervous system-mediated sympathoadrenal discharge triggered by hypoglycemia.
4. Diabetic Ketoacidosis: DKA is an acute complication of untreated/inadequately treated Type I diabetes caused by profound insulin deficiency. Ketones are eventually burned for energy source instead of glucose causing acidosis. Many patients have DKA when they are diagnosed with type 1 diabetes. Also, lower income can contribute to DKA, as people try to make the insulin they have stretch, so do not receive adequate coverage or do not have the means to buy testing supplies to know where they are with their blood glucose.
5. Hyperglycemia, Hyperosmolar Syndrome: HHS is an acute complication of untreated/inadequately treated Type 2 diabetes. This is more common in the elderly who are treated with medical nutrition therapy only, or medications, but not testing. Usually, the person will have an illness predisposing them to HHS. Severe hyperglycemia leads to severe dehydration. The patient usually has enough of their own insulin circulating to prevent ketosis.
Image used with permission of AllRefer Health http://health.allrefer.com http://medicalimages.allrefer.com/large/low-blood-sugar-symptoms.jpg |